A Radical Shift in Healthcare Management
In a bold move aimed at transforming the healthcare landscape, UK Prime Minister Keir Starmer has revealed plans to abolish NHS England, signaling a profound shift in how the country's healthcare is managed. By pulling the plug on this administrative body, Starmer hopes to cut red tape and direct funds more effectively within the healthcare system.
NHS England, a fixture since 2012, was an outcome of the Conservative-Liberal Democrat coalition. It was designed to function independently while managing services, negotiating contracts, and overseeing budgets. However, Starmer has described its role as an unnecessary duplicate of functions better managed by the government directly, hence his reasoning for merging it back into the Department for Health and Social Care (DHSC).

Meaningful Change or Risky Disruption?
The plan is to integrate NHS England into the DHSC over the next two years, slashing the combined workforce by 50%, from 18,000 to 9,000 employees. While this reorganization touts improved efficiency, it also raises eyebrows among some healthcare professionals and unions who fear such significant changes could disrupt vital services. Critics point to the lengthy 7 million strong waiting lists and chronic staffing shortages as problematic issues that may be exacerbated by such upheaval.
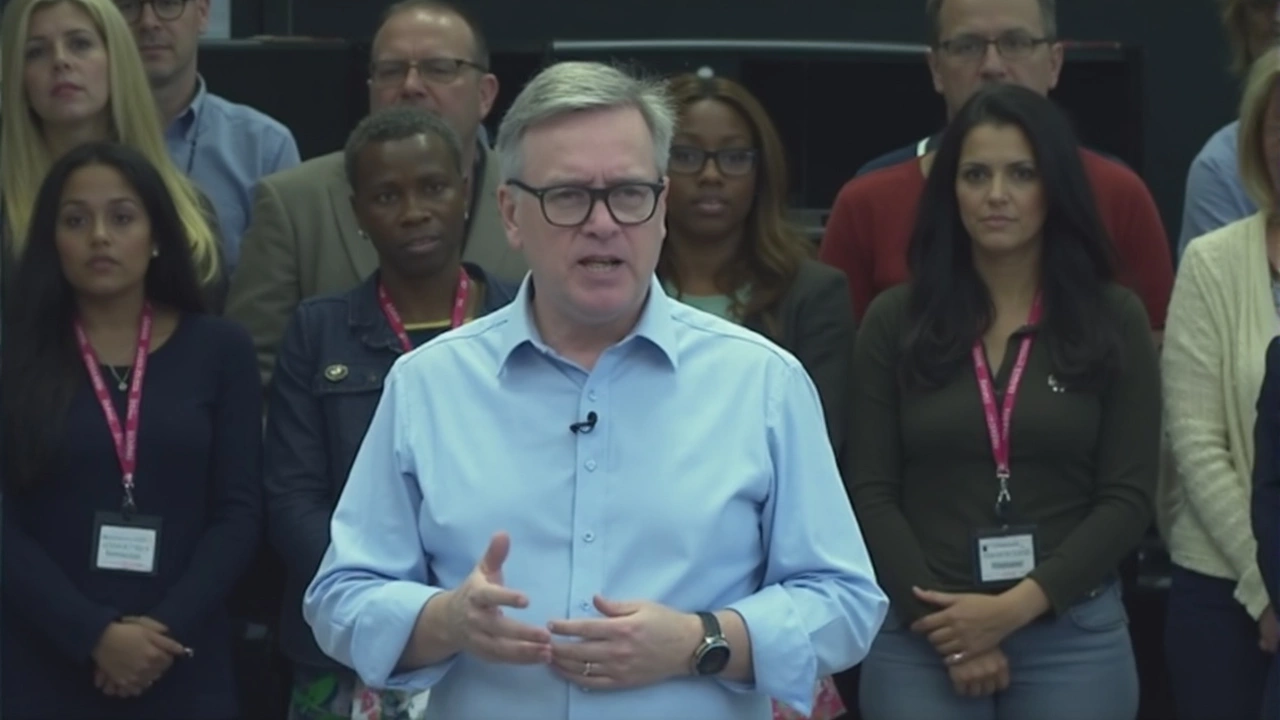
Health Secretary Wes Streeting painted this initiative as a necessary measure to rectify the problematic elements introduced by the 2012 reforms, notorious for resulting in unprecedented patient waiting times and dissatisfaction. He declared this decision as the "final nail in the coffin" for the flawed reorganization.
Proponents argue that re-channelling resources to the frontlines, drastically trimming bureaucracy, and managing the NHS's vast £200 billion budget more effectively are critical priorities.
Even with political support from the Conservatives and Liberal Democrats, the plan faces scrutiny from unions and healthcare workers. They stress that operational challenges require substantive solutions beyond mere administrative changes. The central concern remains: can such a sweeping restructuring truly improve patient care without derailing current services?
As the transition progresses, the healthcare community and the public will closely observe how these changes unfold and what impact they will have on a system already grappling with multiple challenges.




Write a comment